Lumbar Spinal Fusion
What is Lumbar Spinal Fusion ?
Lumbar spinal fusion is a surgical procedure that permanently joins two or more vertebrae in the lower back to improve stability, reduce pain, and prevent excessive movement. It is commonly recommended for conditions such as degenerative disc disease, spinal stenosis, spondylolisthesis, fractures, or chronic lower back pain that has not responded to conservative treatments.
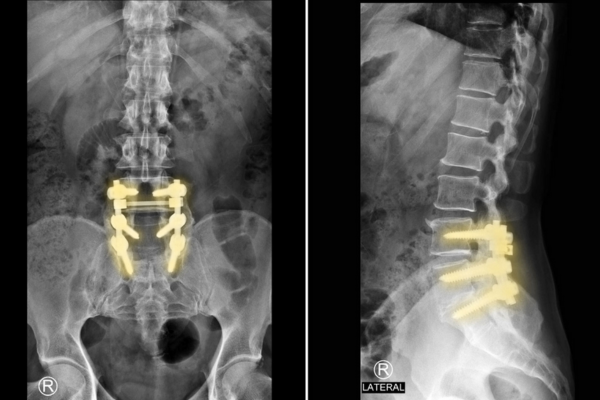
During the procedure, the surgeon places bone grafts or implants between the affected vertebrae, sometimes supported by screws, rods, or plates for additional stability. Over time, the bones naturally fuse, creating a solid structure.Recovery varies, but patients typically require physical therapy and activity modifications for several months.
Indications for Lumbar Spinal Fusion
It is recommended for conditions such as:
- Degenerative Disc Disease – Worn-out discs causing pain and instability.
- Spinal Stenosis – Narrowing of the spinal canal leading to nerve compression.
- Spondylolisthesis – A slipped vertebra causing pain and instability.
- Herniated Disc – Severe cases requiring stabilization.
- Fractures or Tumors – When structural integrity is compromised.
- Failed Back Surgery Syndrome – When previous spine surgery did not provide relief.
Types of Lumbar Spinal Fusion
- Posterior Lumbar Interbody Fusion (PLIF) – Fusion from the back with disc removal and bone graft placement.
- Transforaminal Lumbar Interbody Fusion (TLIF) – Similar to PLIF but with less muscle disruption.
- Anterior Lumbar Interbody Fusion (ALIF) – Performed through the abdomen, avoiding back muscles.
- Lateral Lumbar Interbody Fusion (XLIF/DLIF) – Access through the side to minimize back trauma.
- Minimally Invasive Lumbar Fusion – Uses smaller incisions and advanced techniques for faster recovery.
Procedure Overview
- Anesthesia – The patient is placed under general anesthesia.
- Incision & Access – The surgeon reaches the spine through the back, abdomen, or side.
- Disc Removal & Bone Graft Placement – Damaged disc material is removed, and bone grafts (from the patient, donor, or synthetic) are inserted.
- Implantation of Hardware (if needed) – Screws, rods, or plates may be used for stability.
- Closure & Recovery – Incisions are closed, and the patient is monitored for complications.
Recovery & Rehabilitation
- Hospital Stay: 2–5 days (varies by technique).
- Initial Recovery: 4–6 weeks of limited activity.
- Complete Healing: 6–12 months as the bone graft solidifies.
- Rehabilitation: Physical therapy starts after initial healing to improve mobility and strength.
Potential Risks & Complications
- Infection
- Blood clots
- Nerve damage
- Non-union (failure of bones to fuse)
- Persistent pain
- Hardware-related complications
